WPW
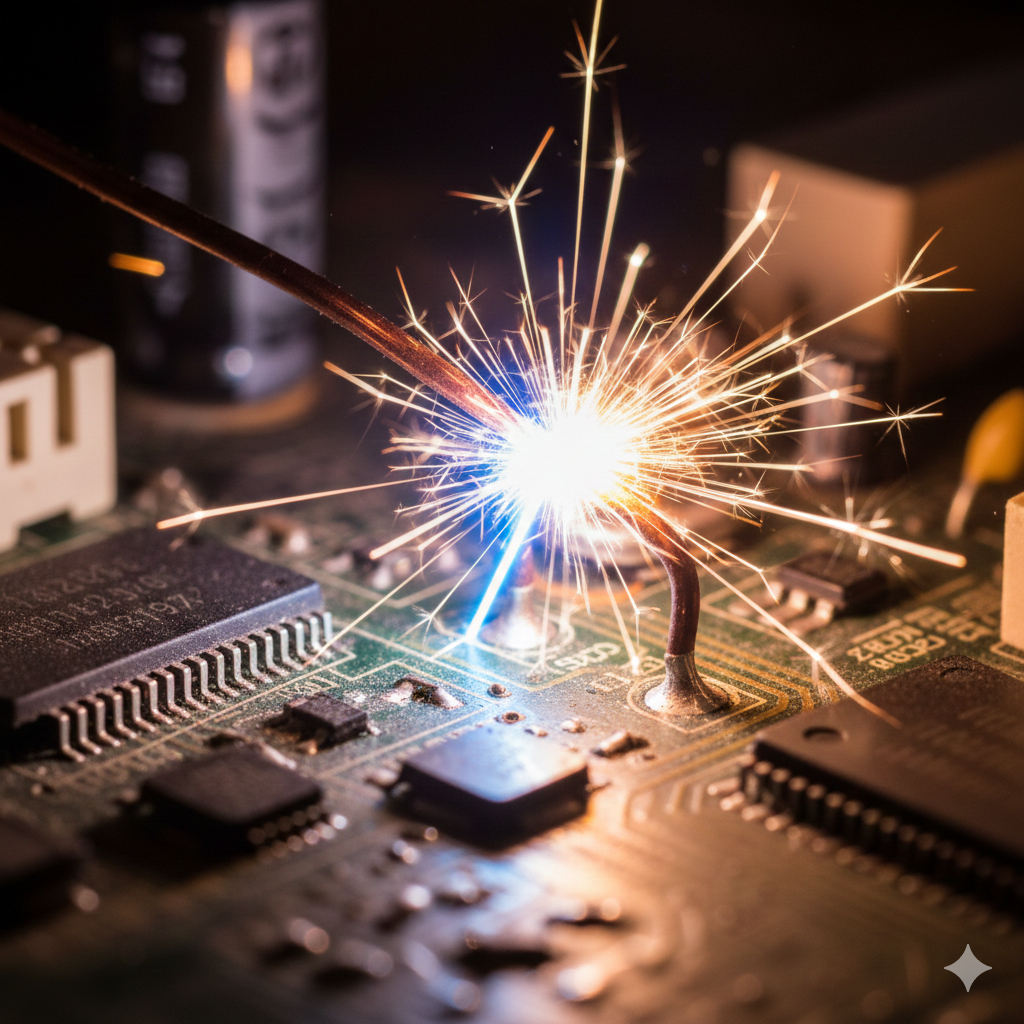
The Short Circuit
In a normal heart, electrical signals travel from the atria to the ventricles through a single pathway called the atrioventricular (AV) node. In WPW syndrome, the accessory pathway acts like a bypass, creating a "short circuit." This allows electrical signals to travel faster than usual or even circle back, creating a fast loop of electrical activation, causing the heart to beat too quickly.
Atrioventricular Re-Entry Tachycardia (AVRT) & Wolff-Parkinson-White Syndrome
-
Wolff-Parkinson-White (WPW) syndrome is a heart condition characterised by an extra electrical pathway between the atria (upper chambers) and ventricles (lower chambers) of the heart. This extra pathway, called an accessory pathway, can cause the heart to beat abnormally fast, leading to episodes of rapid heart rate known as tachycardia.
-
The accessory pathway in WPW syndrome is made of normal heart muscle tissue, similar to the AV node but located in an abnormal position. This pathway can conduct electrical impulses directly from the atria to the ventricles, bypassing the AV node.
-
WPW syndrome is relatively rare, affecting about 1 to 3 in every 1,000 people. It is often congenital, meaning people are born with it, though symptoms may not appear until later in life.
-
An electrocardiogram (ECG) is a key tool in diagnosing WPW syndrome. The ECG may show:
A short PR interval (the time between atrial and ventricular contraction).
A delta wave, which is a slurred upstroke at the beginning of the QRS complex.
Widening of the QRS complex, indicating that the ventricles are being activated earlier than normal and outside of the normal, rapid conduction system.
The location of the delta wave and the direction of the QRS complex can help pinpoint where the accessory pathway is located in the heart.
-
During normal rhythm, the accessory pathway may conduct electrical impulses in the same direction as the normal AV node. The AV node has a built-in delay and then uses a special connection which rapidly conducts the electrical signal through the pumping chambers of the heart. An accessory pathway has no delay, so it conducts to the pumping chambers immediately. It’s not connected to the special rapid connection and usually the wave from the AV node overtakes the accessory pathway signal, so you can see both elements on the ECG.
-
A concealed accessory pathway is an extra pathway that only conducts electrical impulses backward, from the ventricles to the atria. It doesn’t show up on a standard ECG during normal rhythm but can still cause episodes of supraventricular tachycardia (SVT).
-
In WPW syndrome, if atrial fibrillation (a chaotic, irregular heartbeat) occurs, some accessory pathways can conduct impulses very rapidly to the ventricles. This can lead to a dangerously fast heart rate, which may cause ventricular fibrillation - a life-threatening condition that requires immediate medical attention.
-
SVT in WPW syndrome is often due to a circuit involving the AV node and the accessory pathway. Every so often an early heart beat occurs. If the early beat travels down only one of the normal AV node or the accessory pathway, it can return up the other unused pathway, setting up a circular circuit that causes a rapid heartbeat (tachycardia). Symptoms include palpitations, dizziness, fainting or shortness of breath.
-
We assess the risk of an accessory pathway by:
Electrophysiology studies (EPS): This test maps the electrical activity of the heart to identify the pathway and its properties.
Exercise testing: To see if the pathway conducts rapidly during physical activity.
Holter monitoring: A portable ECG device worn for 24 hours or more to detect abnormal rhythms.
If the pathway conducts very rapidly, it is considered high-risk and may require treatment.
-
Catheter ablation is the most common treatment for WPW syndrome. During this procedure:
Thin, flexible tubes (catheters) are inserted into a blood vessel and guided to the heart.
Electrodes on the catheters map the heart’s electrical activity to locate the accessory pathway.
Radiofrequency energy or cryoablation (freezing) is used to destroy the pathway.
Risks of Catheter Ablation
While generally safe, risks include:
Heart block (damage to the AV node, requiring a pacemaker).
Perforation of the heart (rare).
Recurrence of the pathway (in some cases).
-
John Parkinson and Paul Dudley White were British and American cardiologists, respectively, who described the syndrome in 1930.
Louis Wolff was an American cardiologist who contributed to the understanding of the ECG findings.
Note: Dr. James Parkinson, who described Parkinson’s disease, is not the same person as John Parkinson. WPW syndrome is not related to Parkinson’s disease.
-
